What Is Fetal Tachycardia?
Pregnancy, a journey of profound transformation, often prompts parents to seek knowledge and support, especially in the face of unexpected challenges like fetal Tachycardia. This article will discuss fetal Tachycardia, outlining its types, potential causes, and the crucial role that continuous fetal monitoring plays during labour.
Furthermore, it will delve into the legal aspects surrounding the involvement of medical negligence lawyers in cases where fetal monitoring malpractice is suspected.
Understanding Fetal Tachycardia
Fetal Tachycardia is a medical term used to describe an increase in the baseline fetal heart rate (FHR) above 160 beats per minute (bpm). It is categorized into two main levels:
- Mild fetal Tachycardia, with an FHR ranging between 161-180 bpm;
- Severe Tachycardia, characterized by an FHR exceeding 180 bpm for a duration of at least three minutes.
Causes of Fetal Tachycardia
There are several factors that can contribute to fetal Tachycardia, including the following:
Maternal Factors
- Maternal dehydration: Severe maternal dehydration can lead to reduced blood volume and lower oxygen levels in the maternal circulation, which can affect the fetus and lead to Tachycardia.
- Maternal infection or fever: Infections or illnesses causing high maternal fever can directly affect the fetal heart rate, as an elevated temperature triggers a fetal stress response.
- Maternal stress or anxiety: Stress hormones released by an anxious mother might cause a tachycardic response in the fetus.
Fetal Factors
- Fetal Hypoxia: When the fetus does not receive enough oxygen, Tachycardia develops as a compensatory response.
- Fetal Anemia: Fetal anemia can cause an elevated heart rate as the heart tries to compensate for the blood’s reduced oxygen-carrying capacity.
- Fetal Hyperthyroidism: In rare cases, the fetus may develop hyperthyroidism, a condition in which the thyroid gland produces an excess of thyroid hormones, leading to a rapid heart rate.
Placental Factors
- Placental insufficiency: A poorly functioning placenta may not provide adequate oxygen and nutrients to the fetus, causing Tachycardia.
Umbilical Cord Issues
- Cord compression: Temporary compression of the umbilical cord can reduce oxygen and nutrient flow, causing a transient increase in the heart rate.
Fetal Tachycardia and Medical Negligence
Close attention to the fetal heart strip is a fundamental aspect of prenatal care and labour, as any deviations from a reassuring heart rate pattern may signify a potential for serious birth injuries.
Medical negligence in the context of fetal heart monitoring can manifest in several ways, each carrying the potential for harm to the unborn child:
- Failure to diagnose fetal distress: In cases where doctors overlook non-reassuring patterns on the heart rate strip, a diagnosis of fetal distress might be delayed, potentially jeopardizing the well-being of the fetus.
- Underqualified staff handling monitoring: Sometimes, underqualified or inadequately trained hospital personnel are entrusted with operating fetal heart rate monitors, increasing the risk of misinterpretation and missed critical signs.
- Communication breakdown: Effective communication between healthcare providers is crucial in the context of fetal monitoring. Nurses and other staff members who recognize non-reassuring heart rate patterns must promptly relay this critical information to the attending doctor. Failure to communicate these findings can delay addressing potential fetal distress.
- Medication errors: In some cases, medication may be administered to the mother to address the underlying issue causing fetal Tachycardia. Errors in medication administration, such as incorrect dosages or contraindicated drugs, can harm both the mother and the baby.
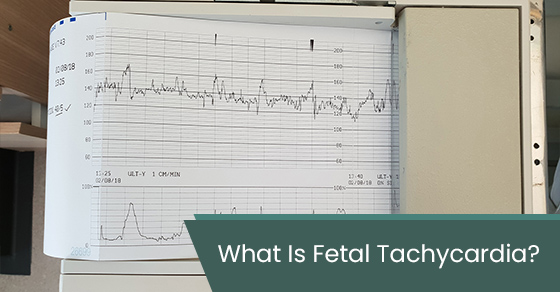
Understanding Fetal Heart Monitoring
Fetal heart monitoring is a critical aspect of prenatal care and labour management. It assists healthcare professionals in tracking the baby’s heart rate and uterine contractions, providing vital insights into the baby’s health and potential concerns.
There are two primary methods for fetal heart monitoring: external and internal. Each technique serves specific purposes and has its own set of advantages.
External Monitoring
This method, utilized throughout pregnancy and labour, involves affixing two sensors to the mother’s abdomen with elastic belts. These sensors employ reflected sound waves (ultrasound) to record the fetal heart rate and contraction duration, subsequently captured by a machine.
Internal Monitoring
Typically initiated during labour after the cervix has dilated to a certain extent and the amniotic sac has ruptured, this method entails securing a sensor to the mother’s thigh.
A thin wire (electrode) is threaded through the cervix into the uterus and attached to the baby’s scalp, precisely monitoring fetal heart rate, contraction strength, and timing.
The choice between external and internal fetal heart monitoring methods allows healthcare providers to obtain the most accurate and reliable readings. Internal monitoring, for example, is less affected by external factors, offering precise data that is invaluable for making informed decisions during labour and childbirth.
Fetal heart monitoring enables early detection of potential issues, provides valuable data for treatment adjustments, and ensures that childbirth proceeds safely and smoothly.
The Outcomes of Failing to Address Fetal Tachycardia
When healthcare providers fail to recognize fetal Tachycardia in prenatal care or during labour and delivery, it can result in various outcomes depending on the cause and when diagnosis or treatment occurs. Some potential repercussions of overlooking fetal Tachycardia include the following:
- Labour and delivery complications: During labour, fetal Tachycardia may signal distress, and failure to address it promptly can result in delivery complications, potentially requiring an emergency cesarean section.
- Cardiovascular strain: Prolonged Fetal Tachycardia can strain the developing fetal heart, possibly causing cardiovascular failure. The fetal heart is remarkably adaptable, but sustained high heart rates can exhaust it, impairing blood circulation and oxygen/nutrient delivery to vital organs, potentially resulting in cardiac dysfunction.
- Nonimmune fetal hydrops: Nonimmune fetal hydrops can result from prolonged Tachycardia, which disrupts fetal fluid balance, causing excess fluid accumulation in body cavities, straining the baby’s cardiovascular system, and leading to severe complications.
Seeking Legal Recourse
When medical malpractice is suspected, consulting with a medical negligence lawyer can help families investigate the situation and determine whether healthcare providers’ actions (or lack thereof) amounted to negligence. An experienced medical malpractice lawyer can assist affected families by:
- Investigating the case: Conducting a thorough investigation to determine if medical negligence occurred and how it contributed to the harm of the baby or mother.
- Collecting evidence: Gathering medical records, reports, and expert opinions to support the legal claim.
- Building a strong case: Crafting a compelling legal case by outlining the negligence, the harm caused, and the resulting damages.
- Pursuing litigation: Your medical negligence lawyer can initiate a lawsuit. They will represent your interests in court, presenting your case before a judge or jury.
- Pursuing compensation: Following the case resolution, your lawyer will diligently work to ensure that you are rightfully awarded compensation, which may encompass various expenses such as medical bills, rehabilitation costs, lost income, and emotional distress.
Consult With an Experienced Medical Negligence Lawyer
If you or your child has experienced severe injury or harm due to medical error or negligence, seeking expert legal guidance is crucial. Sommers Roth & Elmaleh has been at the forefront of medical malpractice law in Canada for over 40 years. We specialize in medical negligence, making it our sole focus.
Call Sommers Roth & Elmaleh at 1-844-940-2386 or contact us online to request a free consultation. Our dedicated team of medical negligence lawyers is ready to listen, evaluate your case, and provide the legal support and guidance you need.
Disclaimer and Liability Exclusion
The information on this page is provided for general information purposes only. It should not be construed as legal advice. It does not constitute legal or other professional advice or an opinion of any kind. Readers should seek specific legal advice regarding any specific legal issues. We do not in any way guarantee or warrant the accuracy, completeness or quality of the information on this page. The posts on this page are current as of their original date of publication, but they should not be relied upon as timely, accurate or fit for any particular purpose.
Accessing or using this web site or the content herein does not create a lawyer-client relationship.
This page may contain links to third party web sites. We are unable to, and do not, monitor and guarantee the quality of the information disseminated and accessible through those links, which are provided for convenience only. We do not endorse the information contained in linked web sites nor guarantee its accuracy, timeliness or fitness for a particular purpose.